Abstract
INTRODUCTION: HCT is a potentially curative treatment option for high-risk hematologic malignancies. Approximately 20,000 HCTs are performed in the US annually. A wide range of costs for both autologous HCT (auto-HCT) and allogeneic HCT (allo-HCT) are reported. For commercially insured patients with hematologic malignancies, the economic burden of an auto-HCT was estimated at $390,159 and allo-HCT at $745,341 in 2011-2014 over a 6-month pre- and 12-month post-HCT period (Bonafede 2017), indirect and caregiver costs may further increase burden (Applebaum 2017; Denzen 2017). We characterize all-cause healthcare resource utilization (HRU) and costs among commercially insured patients with hematologic malignancies who received an auto- or allo-HCT in a more contemporary era.
METHODS: Adults with hematologic malignancies and ≥1 inpatient admission for an auto- or allo-HCT (Jan 2015-Mar 2020) were identified from the MarketScan Commercial and Medicare Supplemental Databases. Patients were indexed on the date of first HCT inpatient admission. Included patients had 12 months of continuous enrollment before and after the index date and ≥2 medical claims with a diagnosis code for an eligible hematologic malignancy (acute myeloid leukemia, myelodysplastic syndrome, myelofibrosis, myeloproliferative disease, acute lymphoblastic leukemia, chronic myeloid leukemia, multiple myeloma, Hodgkin disease, or lymphoma) with ≥1 claim occurring on or before the index date. Patients with an HCT prior to the index date were excluded. Controls were selected from patients meeting study criteria with the exception of an HCT claim requirement. The index date for patients in the control group was randomly assigned based on the time between diagnosis and HCT for the HCT cohorts. Controls and HCT recipients were matched 3:1 based on age, sex, insurance type, Deyo-Charlson Comorbidity Index categories, and hematologic malignancy. Total all-cause HRU and inpatient, outpatient (ie, ED [emergency department], physician office, other visits), and pharmacy costs were compared between the HCT cohorts and controls over the 6-month pre- and 12-month post-index periods. Healthcare costs (2021 US$) were based on paid amounts of adjudicated claims, including insurer/health plan payments and patient cost-sharing (copayment, deductible, and coinsurance).
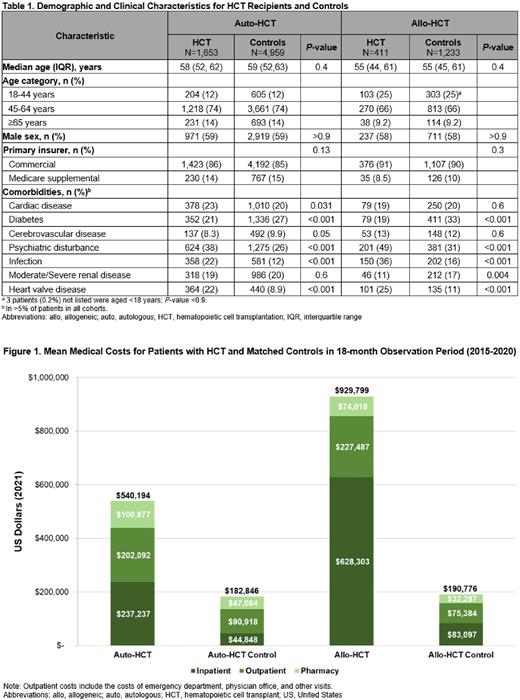
RESULTS: A total of 1653 auto-HCT recipients were matched to 4959 controls and 411 allo-HCT recipients matched to 1233 controls. After matching, HCT cohorts and controls were similar in age, sex, insurance type (Table 1), Deyo-Charlson Comorbidity Index categories, and hematologic malignancy. Pre-index comorbidities differed among the HCT and control cohorts, with psychiatric disturbances, infections, and heart valve disease significantly more common in both the auto- and allo-HCT recipients vs matched controls (P<0.001 for all). Multiple myeloma was the most common eligible indication for auto-HCT whereas acute myeloid leukemia/myelodysplastic syndrome/myelofibrosis/myeloproliferative disease were the most common indications for allo-HCT. Over the 18-month observation period, total all-cause costs were significantly higher for auto-HCT recipients vs matched controls ($540,194 vs $182,846; P<0.001; Figure 1), with auto-HCT recipients having significantly higher costs than controls for all categories evaluated except ED visits during the post-index period ($817 vs $879; P<0.4). Auto-HCT costs were driven by inpatient and outpatient costs. For allo-HCT recipients vs matched controls, total all-cause costs were significantly higher ($929,799 vs $190,776; P<0.001) during the 18-month observation period, with allo-HCT recipients having significantly higher costs than controls for all categories evaluated except ED visits during the pre- and post-index periods ($568 vs $533; P=0.11, $824 vs $862; P>0.9). Inpatient costs were the primary cost driver for allo-HCT recipients.
CONCLUSIONS: The use of HCT, a potentially curative treatment for some patients with hematologic malignancies, is associated with considerable HRU and economic burden. This analysis did not include indirect costs, caregiver burden, or donor costs, and therefore likely underestimates the true burden of HCT for patients with hematologic malignancies.
Disclosures
Narkhede:ADC Therapeutics: Membership on an entity's Board of Directors or advisory committees; EUSA pharmaceuticals;: Research Funding; Gilead/Forty-seven: Research Funding; Gilead: Research Funding; Roche: Research Funding; Genetech: Research Funding; Genmab: Research Funding; TG Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Seagen Inc.: Research Funding. Liu:Seagen, Inc: Current Employment, Current equity holder in publicly-traded company. Surinach:Seagen, Inc: Consultancy. Fanale:Seagen, Inc: Current Employment, Current equity holder in publicly-traded company. Yu:Seagen, Inc: Current Employment, Current equity holder in publicly-traded company. Winter:Seagen, Inc: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees; OncLive: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal